Table of Contents
Most babies are positioned head down and legs up in the womb before birth. Delivering this way is typically easier and is medically termed ‘cephalic’ presentation or position.
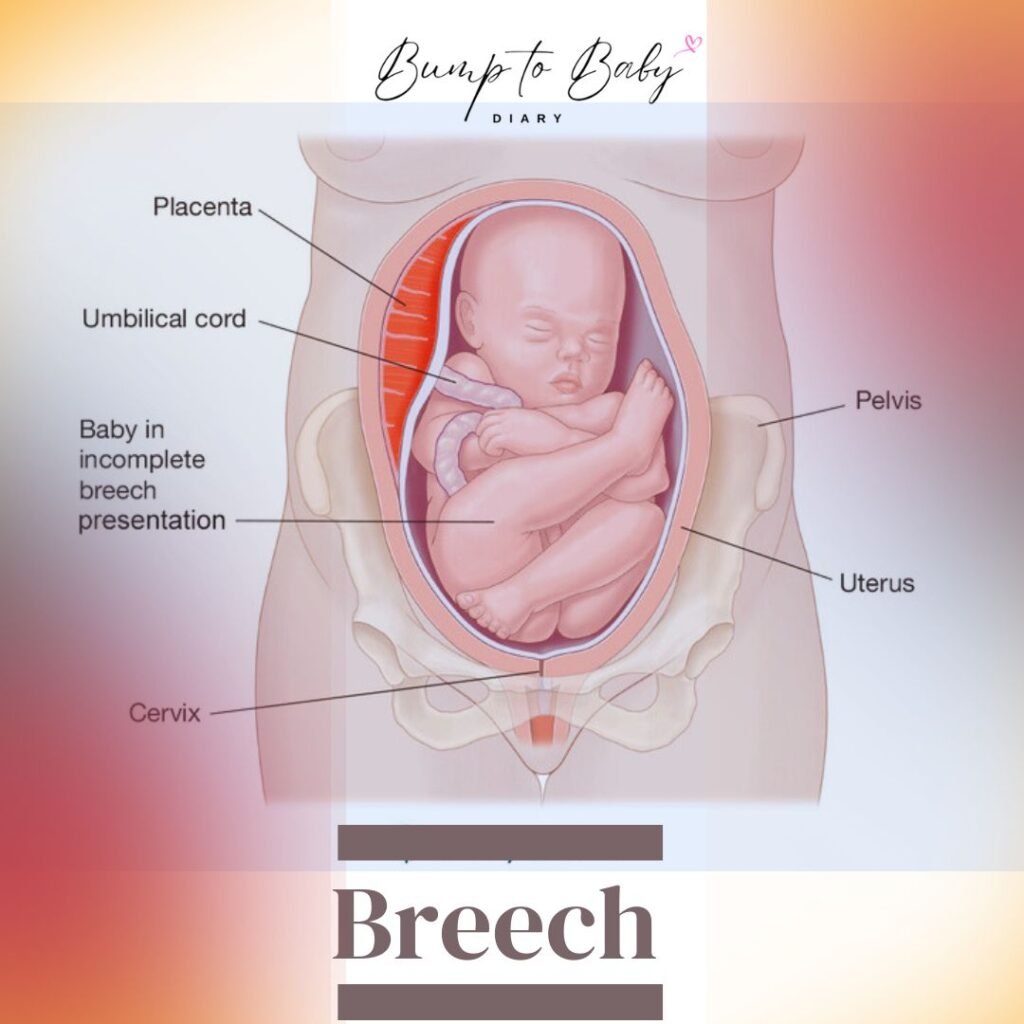
In certain instances, the baby ends up in the opposite position in the womb, with the hip or leg down and the head up. This position, known medically as the ‘breech’ position, may necessitate special delivery arrangements. This article discusses the causes of breech presentation, how to recognize it, associated risks, and appropriate actions.
How Common Is The Breech Position?
Babies born after 39 weeks of gestation, termed ‘full term’, may experience breech position in 3–4 out of every 100 cases. Premature babies have a higher likelihood of being born in breech position.
For instance, approximately 7 out of 100 babies delivered at 32 weeks of pregnancy are expected to be in the breech position. This likelihood increases to about 25 percent for babies born at 28 weeks or earlier, meaning 1 in 4 babies is born in the breech position.
Moreover, if a baby was born with breech presentation in a previous pregnancy, there’s a chance of recurrence in subsequent pregnancies. If the first child was delivered breech, the likelihood in the second pregnancy is about 10 percent, rising to 27 percent in third pregnancies.
Furthermore, if a baby was delivered via cesarean section in a previous pregnancy, the chance of breech presentation in the next pregnancy nearly doubles.
Reasons for Baby's Breech Position
The exact cause of breech position isn’t always clear, but certain factors may increase the likelihood, including:
- Previous pregnancies
- Carrying twins or multiples
- Abnormal levels of amniotic fluid
- Abnormalities in the size or growth of the uterus, such as fibroids
- Placenta previa, where the placenta partially or completely covers the cervix
- Premature birth, occurring before 37 weeks of gestation
- Previous cesarean section or history of a breech delivery
How to Determine if Baby is in Breech Position?
It can be challenging to discern the baby’s position in the womb on your own. Therefore, attending regular antenatal checkups is crucial to ascertain the baby’s position for delivery. During these checkups, the doctor will palpate your abdomen to feel the baby’s position.
Using gentle pressure, the doctor will assess various parts of your abdomen to identify the baby’s head, back, legs, and hips. In the breech position, the baby’s head is positioned upward, while the hips and/or legs are downward, with the baby’s back turned to either side of your body. Additionally, a pelvic exam may be conducted.
If necessary, the doctor may recommend an ultrasound to confirm whether the baby is indeed in the breech position.
What to Do if Baby is in Breech Position?
If the baby remains in the breech position after 36 weeks, your doctor will discuss the following options with you:
- External Cephalic Version (ECV): This procedure involves attempting to rotate the baby from breech to cephalic position by applying gentle pressure on the abdomen. Your doctor will explain the potential benefits, risks, and considerations associated with this procedure.
- Planned Breech Delivery: Your doctor may discuss the possibility of delivering the baby vaginally in the breech position, similar to a normal delivery. They will provide information about the process and potential outcomes.
- Planned Cesarean Section: Your doctor may recommend delivering the baby via cesarean section before the onset of labor pains. They will discuss the advantages of this approach, which is often considered safer than planned breech delivery.
It’s important to note that complications can arise during a vaginal delivery of a breech baby, sometimes necessitating an emergency cesarean section. Therefore, it’s essential to be mentally prepared for potential variations in the delivery plan.
How to Move the Baby from Breech to Normal Position?
If the baby remains in the breech position at 36 weeks of pregnancy, your doctor may attempt to reposition the baby for a normal delivery using a special procedure called an ‘external cephalic version’ (ECV). Typically, this procedure is performed at or after 37 weeks of gestation to minimize the risk of preterm delivery.
Before attempting an ECV, your doctor will assess whether it’s safe for both you and the unborn baby. They will discuss the potential benefits, risks, and considerations of the procedure with you, allowing for informed decision-making.
External Cephalic Version Procedure
During an external cephalic version (ECV) procedure, gentle pressure is applied to the pregnant woman’s abdomen to reposition the baby for normal delivery. This involves bringing the baby’s head down and lifting the legs up. The success rate of this procedure is around 50%.
ECV is a safe procedure that does not involve any incision or surgery. However, the baby may experience some discomfort during the turning process.
It’s essential to note that ECV should only be performed in a hospital or under the supervision of an experienced gynecologist and obstetrician. This ensures prompt intervention in case of any complications for the mother or the baby. Typically, the procedure is conducted near the delivery room or operating theater to facilitate emergency cesarean delivery if needed.
The procedure typically follows these steps:
- Before performing ECV, an ultrasound is usually done to confirm the baby’s breech position. Your heart rate, blood pressure, and the baby’s heartbeat will also be monitored.
- At the start of the procedure, you may receive an injection to slightly relax your uterus, which is safe for both you and the baby. This may cause a temporary increase in heart rate and blood circulation, along with a warm sensation.
- The doctor will then place their hand on your abdomen and, with gentle pressure, attempt to change the baby’s position inside the womb. Sometimes, two people may be required for this step.
- You may experience discomfort or mild pain during the procedure, which typically lasts a few minutes. If you experience significant pain, the doctor will stop the procedure.
- Continuous monitoring of the baby’s heart rate is performed before and after the procedure. If any abnormalities are detected, the procedure will be halted immediately.
- Following the completion of the procedure, another ultrasound is usually conducted to confirm the baby’s new position.
- If your blood group is negative, you may require an injection of ‘anti-D’ and a special blood test after the ECV, as advised by your doctor.
Seek immediate medical advice if you experience any of the following symptoms after an external cephalic version:
- Vaginal bleeding - Stomach ache - Abdominal tightness, cramping, or contractions - Decreased movement of the baby in the womb
When Not to Perform External Cephalic Version
External cephalic version is typically avoided in the following circumstances:
– Multiple pregnancies
– Need for cesarean section for reasons other than breech presentation
– Recent menstrual bleeding
– Abnormal fetal CTG or heartbeat test results
– Fetal health complications
– Certain reproductive system issues in the mother
– Abnormal placental position or placental abruption
– Onset of labor or rupture of membranes (water breaking)
Complications of External Cephalic Version
While external cephalic version generally has few complications, the following may occur in some cases:
– Premature rupture of membranes
– Emergency cesarean section
– Temporary changes in the baby’s heart rate
– Placental abruption
– Vaginal bleeding
– Premature delivery
– Prolapse of the fetal cord
– Rare instances of stillbirth
Domestic Methods
Some individuals believe that adopting specific lying or sitting positions or using particular techniques can help turn a baby from the breech position to the normal position.
For instance, there are beliefs that crawling in bed, walking frequently, shining a torch light on the stomach, or drinking orange juice may encourage the baby to move into the desired position.
However, there is currently no scientific evidence supporting these methods. Therefore, before attempting any such techniques, it’s essential to consult your doctor to determine whether they are safe for both you and the unborn baby.
During a normal delivery of a breech presentation baby, complications can arise if the baby's head gets stuck in the birth canal due to insufficient widening by the rest of the body. This may lead to head or joint injuries, requiring special delivery equipment such as forceps in some cases. Additionally, there's a risk of the baby's pulse or umbilical cord protruding through the birth canal before delivery, potentially reducing blood and oxygen supply to the baby's body and causing serious complications.
If one of the twins has a breech presentation, a planned cesarean section is usually recommended. However, if the first twin's head is down, a vaginal delivery may be attempted, as the birth of the first baby may create space for the second baby to move into the cephalic position. If needed, the doctor can assist in repositioning the second baby.
Most breech babies do not experience long-term problems after birth. However, those in the breech position during the last three months of pregnancy are at risk of developing Developmental Hip Dysplasia, where the hip joints may not form properly. Regular check-ups and tests after birth are important for early detection and treatment if necessary.
ECV is successful in over half of cases, especially if there has been a previous normal or vaginal delivery. However, there is a possibility of the baby returning to the breech position even after a successful ECV. If unsuccessful, the doctor can discuss alternative options or attempt ECV again after a few days.
ECV is generally safe for both the mother and the unborn baby, with a low complication rate. It's typically performed in a hospital setting to allow for immediate access to emergency cesarean delivery if needed. While rare, emergency cesarean delivery may be necessary in about 1 in 200 cases of ECV.